July, 2014
Next (Part II)
By Michael J. Katin, MD
Our system is under attack and may be approaching a critical juncture (junction)? . In January, we discussed that training programs for radiation oncologists may not be able to produce adequate number of physicians skilled both technically and personally to avoid being overwhelmed. A second problem is that the philosophy of medicine, in general, is turning away from intensive intervention for the individual patient, allegedly for the good of the patient population as a whole.
As described in Next, Part I, the number of physicians in training for palliative-related specialties exceeds the number in training for radiation oncology. At the same time, ASTRO has promoted "Five Wise Choices" favoring reduction in the indications for the use of more complex types of radiation therapy to be used in several types of cancer, or even to be used at all. The featured editorial in the Journal of Clinical Oncology from December 20, 2013, is by Patricia Ganz and calls for "Charting a New Course for the Delivery of High-Quality Cancer Care." This refers to the report published by the Institute of Medicine on "Delivering High-quality Cancer Care: Charting a New Course for a System in Crisis."
Perhaps they could have first collaborated on the best way to manipulate words to make different titles, but the conclusion is that too much money is spent on taking care of people's medical problems and new course consists of not doing that any longer. Does this mean that those of us trained in highly-advanced techniques have now become just a nuisance? Fortunately, Pol Pot is no longer with us, but there are other ways to eliminate unwanted professionals. In any event, in only a short time there will remain only a small cadre of radiation oncologists to keep alive our arcane art.
In the short term there are three major threats. First, all physicians will be continually evaluated for performance. There has already been concern that the methodology may be flawed. This will allow evaluators to purge practitioners who are considered not to be in full accord with guidelines of practice. Second, the number of patients to be treated will decrease as criteria for screening are tightened. This will lead to having more persons diagnosed at an advanced stage of disease, reducing the chance of curative therapy. At the same time, treatments that might increase quality of life but not extend survival will be discouraged. Third, efforts will be made to bring all aspects of patient care together with the argument that this will increase efficiency. While this might be true in theory, it is difficult to demonstrate in practice. The concept of the "medical home " was first developed by the American Academy of Pediatrics in 1967 and subsequently extended to apply to grownups. The main accomplishment of the "medical home " seems to have been generation of studies and publications. A review in 2013 located 5,731 abstracts and papers related to this topic, with the final analysis that there were 19 studies and actually assessed effectiveness, with the conclusion that "there is some evidence" of improvement of the care experience for patients and staff and that there may be improvement in care processes and may be associated with reduced emergency department encounters, but that more research is needed.
Granted, similar difficulty in proving favorable outcomes may be made for other programs started in the mid-20th Century, such as the War on Drugs and the War on Poverty. Regardless, there will continue to be efforts to optimize the relationship between the patient and medical practitioners regardless of whether it can be proven to work better that the admittedly chaotic system that we know and love.
Can we foresee that in the near future radiation oncologists will be living with other physicians in a literal medical house, similar to today's firehouses, in which one is totally committed to the practice and always available, without concern for expenses (since everything is supplied) and also without concern for income, since there won't be any opportunity to spend anything anyway. Finally, all patient care will be coordinated by somebody else, and physicians will be free of any management responsibility....actually, I think we already did that, during residency.
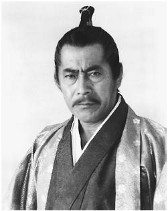
Can there possibly be an alternative for those entering the practice of medicine, let alone radiation oncology, at this point? Yes, there is a precedent. Five hundred years ago there were samurai who became masterless and traveled the countryside offering services for those needing and willing to pay for them Perhaps it is time to break the bonds that restrain us and follow that example*.
*noting that wandering the countryside might be problematic, especially without adequate IT support.