June, 2013
Profiles in Discouragement
By Michael J. Katin, MD
Occasionally it is appropriate to envision the role that radiation oncologists will have in the spectrum of patient care in the future. There is a projection of a severe shortage of physicians in the United States. As efforts are made to recruit intelligent, energetic prospects into the medical profession (at least those who have already decided, for some reason, not to go into law or hedge fund management or a similarly lucrative career ) it would be important to be able to determine how cancer care will be structured by the time they would have completed their training. Unfortunately, our specialty may not exist in twenty years judging from recent developments.
An example: The May 20, 2013, issue of Journal of Clinical Oncology is dedicated to "The Era of Genomics-Driven Cancer Medicine." The consultant editor is Levi Garraway, who has labeled this as "Precision Oncology." It would seem that both precision and accuracy would be important, but we'll let that go for now. Pages 1803 to 1911 contain review articles on molecular profiling and personalized treatment, including setting up the logistics for this as well as, of course, ethical and legal considerations. I noted that in pages 1803 to 1911 there were absolutely zero references to radiation therapy.
It is also to be noted that, prior to the start of the actual scientific content of this journal, there were 131 pages, of which 20 whole pages, three half pages, and one quarter-page were JCO or ASCO-related, 3 were announcement for international meetings, one was a full-page advertisement for the Sarah Cannon Research Institute, and one quarter-page was an announcement for the Dr. Chew Wei Memorial Prize in Cancer Research (C$50,000 to a Canadian who has made outstanding contributions to the treatment, amelioration or cure for cancer; the deadline for nominations is August 30, 2013, 4:00 pm, PDT). Essentially all the other pages are advertisements for pharamaceuticals (not counting the three pages for Sutent at the end of the issue).
It would be hoped that this has nothing to do with the total exclusion in this journal issue of radiation therapy as a treatment option, It would seem to be a matter of time before exome and genome analysis and personally-tailored treatments are the standard of care for cancer patients. How much time? The paper on "Building a Personalized Medicine Infrastructure at a Major Cancer Center" by Meric-Bernstain, Farhangfar, Mendelsohn, and Mills, quotes a reference that it takes 17 years for a new scientific discovery to be used in routine clinical practice, and that there is a success rate of less than 15 per cent. Periodical cicadas also take 17 years to materialize but have a higher success rate. Equally interesting is that despite seminars, board examinations, and advertisements, a substantial percentage of practitioners did not consider EGFR testing in Stage IV lung cancer to be part of the standard evaluation
This may buy us some more time before radiation oncology goes the way of the Yangtze River Dolphin In addition, medical oncologists may have to ask if their main organization is working at cross-purposes. While the JCO devotes an issue to complicated and expensive diagnostic procedures to allow selection of expensive treatments that may not have a high chance of being successful, we are reminded in a report by Mathias and Baker from the May 8 issue of JAMA on "Developing Quality Measures to Address Overuse" that the American Society of Clinical Oncology had recommended against using cancer-directed therapy for patients with solid tumors when there is low performance status, the patient has had no benefit from prior intervention, is ineligible for a clinical trial and there is no strong evidence for the clinical value of further anticancer treatment This recommendation may have as many interpretations as the final episode of "Lost," but there will continue to be a struggle between implementation of new techniques and cost containment.
Obviously, regardless of how rapidly new treatment techniques evolve, both radiation oncology and medical oncology have the nature of their futures threatened by economic factors. May turns out to have been a significant month in terms of publications that produce uncertainly as to the future. The May 23 issue of The New England Journal of Medicine has a "Sounding Board" essay by Steven Schroeder and William Frist for the National Commission on Physician Payment Reform, on "Phasing Out Fee-for-Service Payment." Rarely has a title been more definitive. Steven Schroeder is the chairman of this commission and has had an extremely distinguished career in academia, from Harvard to George Washington University to UCSF to the University of Medicine and Dentistry of New Jersey and now back to UCSF as Distinguished Professor of Health and Health Care and Director of the Smoking Cessation Leadership Center. It is probable that he never was involved in private practice during his distinguished career. William Frist, the honorary chairman, is a cardiac surgeon and former Senate Majority Leader and at one time a potential Presidential candidate (Frist in war, Frist in peace...) He, also, has never been in private practice. In fairness, the article recognizes that developing a fair system of reimbursement is not straightforward. It recognizes that half the nation's health care resources are used by the sickest 5% of patients, but it also implies that procedure-based specialties make too much money compared to those that supply evaluation and management services. There doesn't seem to be the recognition that procedures such as surgery and radiation therapy that could produce cures may be as worthy as providing support for a diabetic patient over many years. It may be true that fee-for-service has a lot of faults, but the entire article loses credibility with Recommendation 11: "Cost-saving measures to offset the elimination of the SGR should come not only from reduced physician payment but also from the Medicare program as a whole. Medicare should also look for savings from reductions in inappropriate utilization of Medicare services." It goes on to say that the $138 billion needed to offset elimination of the SGR "can be found entirely by reducing overutilization of medical services within Medicare." This assumes that the SGR was a good idea in the first place, and this legendary pile of money that will materialize from cracking down on Medicare overutilization has not seemed to have been located after years of searching.
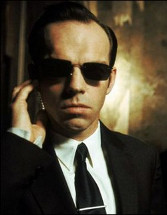
Our specialty is therefore threatened by misdirected efforts at cost containment. The medical oncologists need also be concerned by this. Should we be equally in fear that radiation therapy will be supplanted by sophisticated personalized precision cancer treatment? The medical oncologists need be wary that this could be a Pyrrhic victory for them. From "2001: A Space Odyssey " to "The Terminator " to "The Matrix l," a legitimate fear has been raised. Imagine that diagnosis can be made by such techniques as computerized analysis, currently called 'computer-aided' detection as an ego-saving concession to the radiologist.. A biopsy could be done robotically Tissue can be subjected to molecular profiling, which will then allow selection of the appropriate treatment agent. At that point, what is it that any oncologist contributes, except to get in the way?.
So much for the physician presence issue! Don't tell CMS!!!!!!!!!