September 2010
Trial and Error
By Michael J. Katin, MD
"Learn to get in touch with the silence within yourself, and know that everything in life has purpose.
There are no mistakes, no coincidences, all events are blessings given to us to learn from."
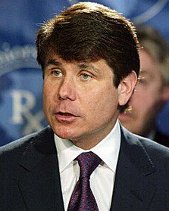
-- Elizabeth Kubler-RossOn August 17, a jury convicted former Illinois Governor Milorad "Rod" Blagojevich on one of twenty-four counts on which he had been indicted related to corruption, perjury, bribery, racketeering, and failure to yield the right of way. This immediately resulted in U. S. Attorney Peter Fitzgerald's vowing to proceed with a retrial on the twenty-three other counts and Governor Blagojevich's asking for an appeal on the one conviction. It is estimated that the trial cost taxpayers somewhere between twenty and thirty million dollars, including $67,463.32 more for payments, reimbursements, and feeding of the jurors,who had been unable to unanimously agree on 95.83% of the charges.
The expense and lack of definitive outcome of this trial is somewhat reminiscent of many clinical trials in medical research. It is probable that not all investigational trials in cardiology, endocrinology, and neurology are done flawlessly and are at risk for improper conclusions resulting from data dredging, false causality, and other creative techniques. Findings in clinical trials can be selectively withheld, such as in the cases of paxil and vytorin. Maybe we shouldn't hold the field of oncology to a higher standard, except for the fact that we have to work with the results every day. It was disheartening to see the report from the Institute of Medicine in April about the status of clinical trials in the United States: Scientists and medical researchers conduct clinical trials to test whether a new product works as expected and is effective at treating disease. Clinical trials with patients suffering from a specific condition represent the crucial link between scientific discovery and medical utility. However, many barriers impede the effectiveness of clinical research in the United States. Planning and executing a clinical trial can take years and cost hundreds of millions of dollars. Our nation's clinical trial infrastructure is not well developed; clinical trials must be conducted in a "one-off" manner, in which substantial resources -- such as funding, investigators, administrators, and patients -- are used for only a finite period of time and then disbanded. Also, clinical trial sponsors, investigators, and research institutions face significant regulatory and administrative hurdles. Finally, patients and providers often do not participate in clinical research in sufficient numbers to support the science, and this problem is compounded by the general of lack of public understanding the value of clinical research and its direct link to improvements in health care.
Although this seems to apply to clinical research in general, the report was commissioned by the National Cancer Institute. The New York Times called attention to this publication in an editorial on April 24 and included reference to the finding that 40 per cent of all clinical trials of the NCI are never completed . This suggests that the Stimulus Program may have been in effect long before it was available elsewhere.
Many leaders in the field of oncology have made recommendations regarding how to address this situation, notably Bruce Chabner, Douglas Blayney, and Allen Lichter, in responses to the New York Times, and Robert Young in The New England Journal of Medicine. Dr. Young called attention to the fact that comments very similar to those of the Institute of Medicine were made in 1997 in the Armitage Report, in 1910 in the Flexner Report, and in 1777 in the Articles of Confederation. It also should be mentioned that with the exception of Dr. Chabner's comments, the solutions involved throwing a lot more money at the problem.
While we wait for a panels of experts to solve the overall clinical trial crisis, attention should be directed to the battlefront at which it all starts: the Phase I trial. Often this is the all-or-none effort to show that a potential new agent can be used in the human, since if excessive toxicity is found then this particular compound can wind up back at the end of the line for additional testing. Although effectiveness is not supposed to be a part of Phase I testing, it is always very encouraging to see this as well. This is particularly the case when a patient is treated based on the context of vulnerability. This is not the title of the next James Bond film, but refers to directing the patient to a Phase I study using a drug that should be effective based on the characteristics of that person's tumor. This should therefore be expected to streamline the progress of a new drug through the clinical trials process and make it available as rapidly as possible to patients. The Karnofsky lecture at this year's American Society of Clinical Oncology annual meeting was delivered by Dr. Daniel von Hoff, who titled his presentation "The Last 12 Weeks." The significance of that title was not to be used as a sequel to "28 Days Later" but as a reference to the requirement of most Phase I trials that patients have a life expectancy of at least 12 weeks. Interestingly, it took approximately 12 weeks (April 20 to July 15) for the Deepwater Horizon gusher to be capped, but otherwise 12 weeks would not seem to be a long time.
Unless you were following the Blagojevich trial, which went from June 3 to August 17 -- nine days short of 12 weeks. Coincidence?